Medical legal and ethical issues chapter 3 – Embarking on a journey through Chapter 3 of Medical Legal and Ethical Issues, we delve into the intricate interplay between medical practice, legal frameworks, and ethical considerations. This chapter explores the complexities that healthcare professionals face, guiding us through the legal implications of medical malpractice, the ethical dilemmas surrounding end-of-life decisions, and the delicate balance between patient rights and professional accountability.
As we navigate this chapter, we will examine the legal and ethical principles that govern medical practice, exploring the concept of informed consent, the duty to maintain confidentiality, and the mechanisms for ensuring professional responsibility. By understanding these essential elements, we empower ourselves to make informed decisions and uphold the highest standards of ethical conduct in the medical field.
Legal Considerations in Medical Practice
Medical practice is governed by a complex legal framework that includes laws, regulations, and ethical guidelines. These legal considerations aim to protect patients, ensure the quality of medical care, and establish standards of conduct for healthcare professionals.
Medical Malpractice
Medical malpractice occurs when a healthcare professional breaches their duty of care to a patient, resulting in injury or harm. To establish medical malpractice, the patient must prove that:* The healthcare professional owed them a duty of care.
- The healthcare professional breached that duty of care.
- The breach of duty caused the patient’s injury or harm.
- The patient suffered damages as a result of the injury or harm.
Common Legal Issues in Medical Practice
Some common legal issues in medical practice include:* Informed consent: Patients have the right to make informed decisions about their medical care. Healthcare professionals must provide sufficient information about the risks and benefits of treatments to obtain valid consent.
Confidentiality
Healthcare professionals have a duty to maintain the confidentiality of patient information. Exceptions exist, such as reporting child abuse or imminent harm to others.
Negligence
Negligence occurs when a healthcare professional fails to meet the standard of care expected of a reasonably prudent professional in similar circumstances.
Ethical Issues in Medical Practice
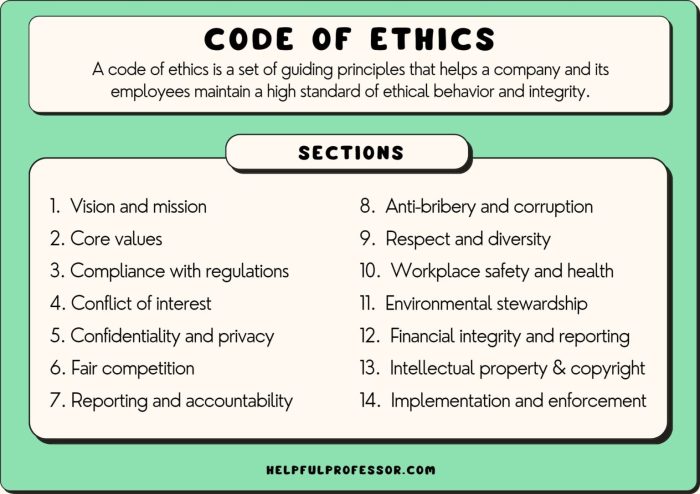
Medical ethics are principles that guide healthcare professionals in making decisions about patient care. These principles include:* Beneficence: The duty to do good and benefit the patient.
Non-maleficence
The duty to do no harm.
Autonomy
The patient’s right to make decisions about their own medical care.
Justice
The fair distribution of healthcare resources.
Ethical Dilemmas in Medical Practice, Medical legal and ethical issues chapter 3
Healthcare professionals often face ethical dilemmas, such as:* End-of-life decisions: Decisions about life-sustaining treatments when a patient is terminally ill.
Organ transplantation
The allocation of organs for transplantation and the ethical considerations surrounding organ donation.
Genetic testing
The implications of genetic testing for patients and their families, including privacy concerns and the potential for discrimination.
Professional Responsibility and Accountability
Healthcare professionals have a responsibility to provide competent care and maintain ethical standards. Professional organizations play a role in setting standards of practice and enforcing ethical guidelines.
Mechanisms for Accountability
Mechanisms for accountability include:* Peer review: The evaluation of a healthcare professional’s practice by colleagues.
Licensing boards
Government agencies that regulate the practice of medicine and discipline healthcare professionals who violate ethical or legal standards.
Disciplinary actions
Sanctions imposed on healthcare professionals for misconduct, including suspension or revocation of their license.
Patient Rights and Informed Consent: Medical Legal And Ethical Issues Chapter 3

Patients have certain rights in medical settings, including:* Right to informed consent: The right to make informed decisions about their medical care after receiving sufficient information about the risks and benefits of treatments.
Right to privacy
The right to have their medical information kept confidential.
Right to access medical records
The right to access their own medical records.
Challenges in Informed Consent
Obtaining informed consent can be challenging in complex medical situations, such as:* Patients with limited capacity: Patients who may not fully understand the risks and benefits of treatments.
Emergencies
Situations where there is not enough time to obtain informed consent.
Treatment refusal
Patients who refuse recommended treatments for personal or religious reasons.
Confidentiality and Privacy
Healthcare professionals have a legal and ethical obligation to maintain patient confidentiality. Exceptions to the confidentiality rule include:* Reporting child abuse or neglect.
- Reporting imminent harm to others.
- Complying with court orders or subpoenas.
Protecting Patient Privacy in the Digital Age
The digital age poses new challenges to patient privacy. Healthcare professionals must implement appropriate measures to protect patient information, such as:* Using secure electronic health records.
- Encrypting patient data.
- Limiting access to patient information.
FAQ Resource
What is the significance of informed consent in medical practice?
Informed consent empowers patients by ensuring they fully understand the risks and benefits of medical procedures before making decisions about their own care.
How does the legal framework protect patient confidentiality?
Legal frameworks impose a duty on healthcare professionals to maintain the privacy of patient information, with exceptions only in cases where there is an imminent threat to others or a legal obligation to report certain conditions.
What is the role of professional organizations in upholding ethical standards in medicine?
Professional organizations play a crucial role in setting standards of practice, providing guidance on ethical issues, and enforcing ethical guidelines through peer review and disciplinary actions.